Understanding PFO and Its Clinical Significance
Patent Foramen Ovale (PFO) is a small opening between the atrial chambers of the heart that fails to close after birth in about 25% of the general population. For most, it remains benign. However, in patients with cryptogenic stroke—strokes without a known cause—PFO is present in nearly 43% of cases, a substantially higher prevalence than in the general population.
This condition is particularly concerning because PFO can allow emboli (tiny blood clots or air bubbles) to bypass the pulmonary filtration system and travel directly to the brain, resulting in a paradoxical embolism and ischemic stroke. Identifying PFO in stroke patients is essential for risk stratification and guiding treatment options like medical therapy or percutaneous closure.
The Traditional Challenge of Detecting PFO
Traditionally, PFO detection has relied on transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE). While TEE is often considered the gold standard, it is invasive and cannot accurately assess shunt size during a Valsalva maneuver—a key technique used to provoke right-to-left shunts. Meanwhile, TTE is less invasive but suffers from significantly low sensitivity.
Clinical meta-analysis data confirms this discrepancy:
TTE: Sensitivity 45.1%, Specificity 99.6%
TCD: Sensitivity 96.1%, Specificity 92.4%
Given these performance gaps, TCD ultrasound has emerged as a non-invasive, highly sensitive, and practical alternative for PFO detection.
What Is TCD and How Does It Work?
Transcranial Doppler ultrasound (TCD) uses a 2 MHz low-frequency probe to measure cerebral blood flow velocity through the cranial bone windows, usually via the transtemporal approach. It can assess changes in blood velocity in major intracranial arteries and detect microembolic signals in real time.
NeurSignal’s NG2 system automates this process with robotic probe positioning and AI-powered signal acquisition. It captures and interprets cerebral blood flow without requiring an expert sonographer, increasing accessibility across clinical settings.
TCD in PFO Detection: The Bubble Study Protocol
The core of PFO detection with TCD lies in the bubble study or contrast-enhanced TCD (cTCD). Here’s how it works:
Contrast Injection: A saline solution mixed with a small amount of air and a bit of the patient’s blood is agitated to form microbubbles and then injected intravenously.
Valsalva Maneuver: The patient performs this maneuver to increase right atrial pressure, which temporarily opens the PFO if present.
Signal Detection: TCD detects high-intensity transient signals (HITS) in the middle cerebral artery, indicating microbubbles that have passed through a right-to-left shunt.
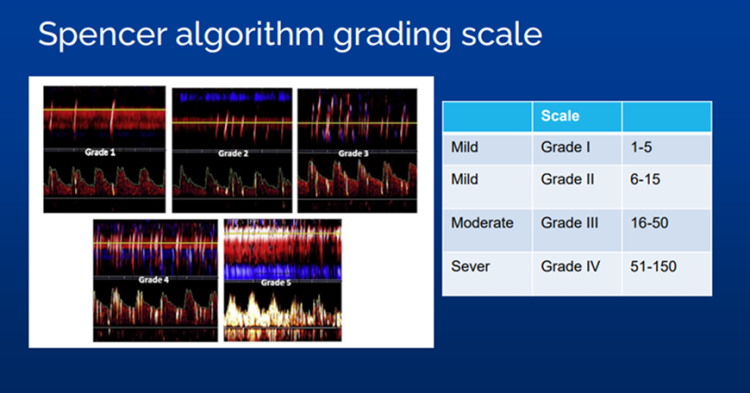
Using this method, TCD can grade the severity of shunting using scales like the Spencer Grading Scale, which ranges from Grade I (1–5 HITS) to Grade V (>100 HITS).
NG2 vs. TTE: Clinical Trial Results That Changed the Game
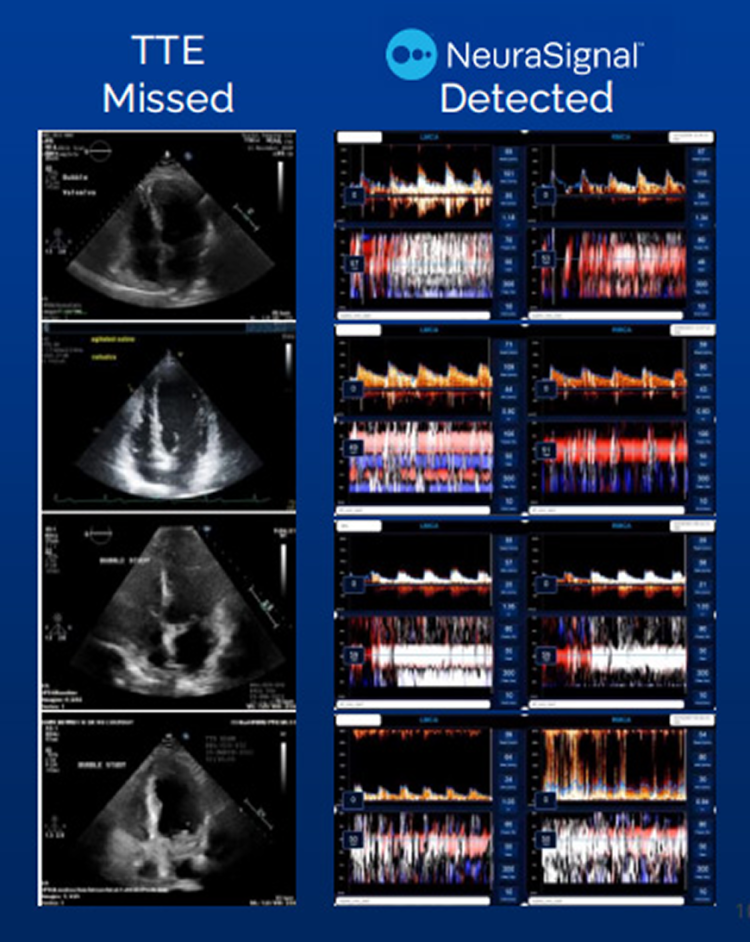
The BUBL Study (ClinicalTrials.gov #NCT04604015) was a multi-site, prospective trial that compared NeuraSignal’s NG2 robotic-assisted TCD against TTE in 129 patients evaluated for embolic stroke or TIA. The findings were remarkable:
NG2 Detection Rate: 63.6%
TTE Detection Rate: 20.9%
Detection of Intervenable Shunts (Spencer Grade ≥3): NG2 27%, TTE 10%
Furthermore, TTE completely missed 18 out of 35 cases with intervenable shunts that NG2 identified.
What makes this even more impressive is that all NG2 exams were performed by non-TCD experts, proving that its AI and automation bridge the skill gap traditionally required for TCD.
Why Valsalva Matters—and Why TEE Falls Short
A key differentiator for TCD over TEE is its compatibility with the Valsalva maneuver. Because TEE requires sedation and involves inserting a probe down the esophagus, patients cannot perform a proper Valsalva during the test. This limitation can lead to underestimation of shunt severity.
In contrast, TCD allows for:
Real-time monitoring during Valsalva
Better quantification of shunt size
More accurate clinical decision-making
One study showed that TEE missed 15% of all shunts, including large ones—highlighting the diagnostic superiority of TCD.
PFO Closure: Evidence That Detection Saves Lives
Recent randomized controlled trials (RCTs) have reshaped the clinical landscape by demonstrating that closing a PFO significantly reduces the risk of recurrent ischemic strokes:
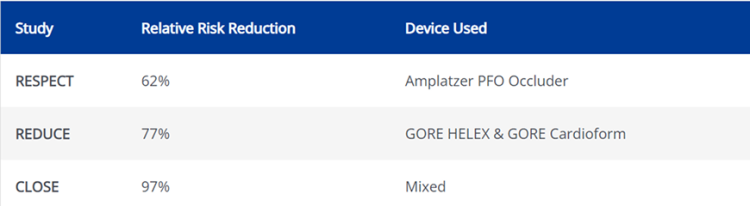
These findings have led to new guideline updates across multiple organizations—including the AAN, ESC, ASA, and ACC—all of which emphasize PFO closure in select cryptogenic stroke patients and support TCD as a first-line diagnostic tool.
Comparative Accuracy: TCD vs. Other Modalities
Let’s break down how TCD compares to TTE and TEE for PFO detection.
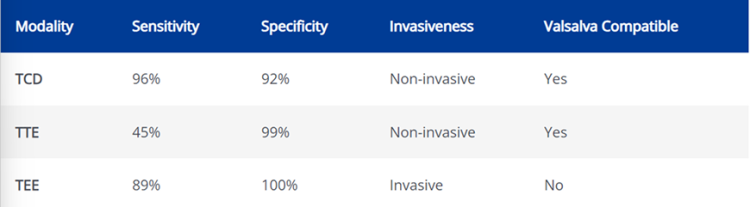
This comparison underscores why TCD, particularly when automated through NG2, is quickly becoming the preferred screening tool.
NG2’s Platform Advantages
NeuraSignal’s NG 2 Intelligent Ultrasound system amplifies the strengths of TCD by offering the following features:
AI-Powered Signal Lock: Locates the middle cerebral artery and locks on in under two minutes.
Guided PFO Exam Workflow: Step-by-step protocol includes bubble injection and real-time Valsalva monitoring.
Automated Shunt Grading: Uses algorithms to identify regions of interest and quantify embolic showers.
Remote Monitoring & Interpretation: Allows stroke teams to review data across facilities or care settings.
Operator Independence: Enables routine use by general healthcare staff without specialized sonography training.
A Case Study: When TCD Makes the Difference
In one clinical example, a 44-year-old man presented with aphasia due to left M1 occlusion. Initial imaging (CTA and TTE) failed to reveal a source. However, TCD revealed a right-to-left shunt. Further testing confirmed the presence of a PFO, allowing timely intervention that would have been missed otherwise.
Such real-world cases reinforce how critical it is to use sensitive, accurate, and rapid diagnostic tools for stroke patients.
What Clinicians Need to Know
For healthcare providers, incorporating TCD into stroke protocols brings several advantages:
Improved Diagnostic Confidence: Especially for cryptogenic stroke cases.
Patient Safety: Avoids the discomfort and sedation risks of TEE.
Efficient Workflow: NG2 reduces exam times and simplifies training.
Better Outcomes: Early detection of large shunts can guide timely closure and reduce recurrence risk.
Moreover, NeuraSignal’s system meets modern telehealth standards, offering secure cloud access, exam alerts, and data integration with PACS and EMR systems.
Growing Recognition in Guidelines
Several prominent organizations now recommend TCD in their stroke and PFO guidelines:
American Academy of Neurology (AAN): Recommends PFO closure and allows TCD as part of the workup.
European Society of Cardiology (ESC): Ranks TCD above TTE for initial RLS screening (Class A evidence).
American College of Cardiology (ACC): Encourages TCD screening before proceeding to TEE.
American Heart Association/American Stroke Association (ASA/AHA): Acknowledges TCD’s ability to detect intra- and extracardiac shunting and improve patient comfort.
TCD as the Future of PFO Detection
Transcranial Doppler ultrasound—especially in its robotic-assisted, AI-enhanced form via NG2 Intelligent—is changing the paradigm of stroke diagnostics. With superior sensitivity, non-invasiveness, and compatibility with physiological maneuvers like Valsalva, TCD is fast becoming the most effective tool for identifying PFO and guiding interventions that save lives.
As the evidence grows and guidelines evolve, TCD is poised to become a routine part of stroke workups, particularly for younger patients and those with cryptogenic stroke. Healthcare systems, practitioners, and patients alike stand to benefit from its wider adoption.